Why you’re asked about ‘conflicting documentation’
07 Jun 2020Don’t call the same condition different things!
By: Robben Morin, clinical documentation specialist
Providers sometimes wonder why they receive queries for conflicting documentation when they believe they have clearly documented the correct diagnosis and associated treatment plan. I’ve received this very question from providers, via their query reply.
Here’s a good definition of conflicting documentation:
“Conflicting documentation occurs when health care providers call the same condition different things. When none of the documented conditions are clearly ruled out by the physician, coders may ask for the most appropriate diagnosis.”
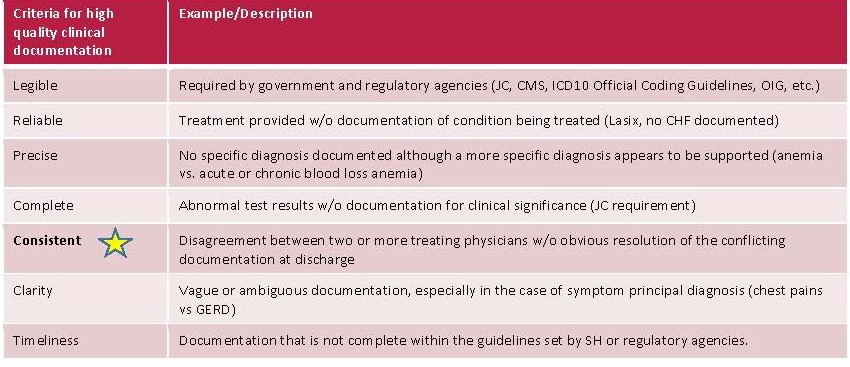
I hope this information on CDI team guidelines is helpful. Below you will find the documentation expectations and criteria for high quality clinical documentation recognized by government and regulatory agencies such as Joint Commission, CMS, ICD10 Official Coding Guidelines, OIG.
- Criteria can be found under “What to Query?” in the 2019 update Official Coding Guidelines: Guidelines for achieving a compliant query process.
- Consistent: Conflicting Documentation falls under this criteria. Examples include but are not limited to:
- Discrepancies between the physical exam and the rest of the documentation, i.e. A&O x3 in physical exam but assessment states acute encephalopathy.
- Consults indicate one diagnosis while the attending states another, i.e. attending documents TIA and requests a neuro consult. Neurologist documents CVA but the attending gives no further documentation regarding the patient’s dx.
- Discrepancy between a diagnosis listed as history, but treatment still being continued during the admission.
Please remember: We are here to help providers improve their clinical documentation through the query process. Whenever a query is sent, it is to clarify documentation found in the medical record that needs the current primary provider to address the conflicting documentation via the query process, and document their medical opinion in the query reply and their clinical chart notes.
Documentation queries (referred to as “queries” in this Practice Brief) are used by coding professionals, CDI professionals, and all professionals responsible for documentation clarification or who have oversight and/or involvement in the query process. Queries continue to be a mechanism to increase the precision of clinical documentation, which translates into accurate clinical data, reflecting a provider’s intent and clinical thought process in a manner that results in an accurate depiction of patient complexity within each episode of care.”
Graph and examples above provided by Melissa Rodriguez, CCS, CCSP, CDIP, CPMA, Clinical Documentation and Coding Specialist, HIM-CDI, Salem Health/West Valley – used by permission
References and credit to:
Guidelines for Achieving a Compliant, Query Practice (2019 Update), It (2019 update) was created through a joint effort of ACDIS and the American Health, Information Association (AHIMA) ACDIS Position Paper: https://acdis.org/system/files/resources/CR-1434%20ACDIS%20AHIMA%20query%20practice%20position_paper.pdf
Ethical Standards for Clinical Documentation Improvement (CDI) Professionals (2016). http://bok.ahima.org/doc?oid=301868#.Xqi6r_6WyUk
Clinical Documentation Improvement, Principles and Practice by Pamela Carroll Hess, MA, RHIA, CCS, CDIP, CPCM; AHIMA Press 2015,
Above information presented by:
Melissa Rodriquez CCS, CCSP, CDIP, CPMA Clinical Documentation and Coding Specialist, HIM-CDI
Salem Health/West Valley, Coder/CDI Roundtable Presentation 4/29/2020