The two main types of sleep apnea and how to treat them
Have you been accused of loudly snoring? Do you ever have a choking or gasping sensation during sleep? Do you wake up feeling fatigued even after a full night’s sleep? If so, you may have sleep apnea.
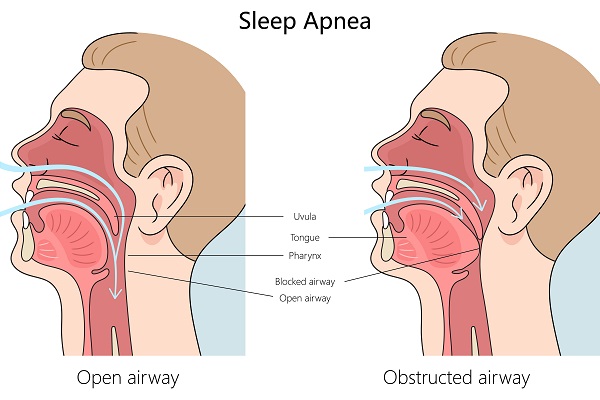
Apnea is Greek for “without breath.” Sleep apnea is a potentially serious sleep disorder, where breathing repeatedly stops and starts during sleep.
There are two main types of sleep apnea:
- Obstructive sleep apnea is the more common type that occurs when the throat muscles relax.
- Central sleep apnea occurs when your brain does not send the right signals to the muscles that control breathing.
Some people have complex sleep apnea, which is a combination of the two.
Risk factors
Sleep apnea affects people of all ages but is twice as common in men than in women. Excess body weight and large neck size also increase the risk. Studies have linked sleep apnea to high blood pressure, increased risk of heart attack, stroke and irregular heartbeat.
Signs and symptoms
The signs and symptoms of OSA and CSA overlap, occasionally making the type of sleep apnea difficult to determine.
The most common signs and symptoms of obstructive and central sleep apnea include:
- Excessive daytime sleepiness (hypersomnia)
- Observed episodes of not breathing during sleep
- Loud snoring
- Morning headache
- Abrupt awakenings with shortness of breath
- Awakening with a dry mouth or sore throat
- Difficulty staying asleep (insomnia)
Treatment
Your doctor may recommend lifestyle changes for milder forms of sleep apnea. That could include measures such as losing weight or quitting smoking to improve symptoms. If your apnea is moderate to severe, a few treatment options are available. Certain devices can open up a blocked airway. Another choice would be an oral appliance. In other cases, surgery may be necessary.
Continuous positive airway pressure (CPAP)
This treatment involves wearing a pressurized mask over your nose while you sleep. The mask is attached to a small pump that creates positive pressure and keeps your airway from collapsing.
It is important to use the device as directed. If you are not comfortable with your mask or the pressure seems too strong, call you sleep physician so that adjustments can be made.
Bilevel positive airway pressure (BIPAP)
Bilevel devices build to a higher pressure when you inhale and decrease to a lower pressure when you exhale. This treatment will boost the weak breathing pattern of central sleep apnea.
Some bilevel devices can be set to automatically deliver a breath if the machine detects you have not taken a breath after a set number of seconds.
Adaptive servo-ventilation (ASV)
The form of positive airway pressure is for patients with central and complex sleep apnea. The machine monitors your normal breathing pattern and stores the information into a built-in computer.
After you fall asleep, the device uses pressure to normalize you breathing pattern and prevent pauses in your breathing.
Surgery or other procedures
The goal of surgery for sleep apnea is to remove excess tissue from your nose or throat that may be causing you to snore, or that may be blocking your upper airway, thereby causing sleep apnea.
Surgical options may include:
Uvulopalatopharyngoplasty (UPPP)
In this procedure, your surgeon removes tissue from the rear of your mouth and top of your throat. Your tonsils and adenoids are usually removed as well. This type of surgery may be successful in stopping the tissue in your throat from vibrating (snoring).
Maxillomandibular advancement
During this procedure, the upper and lower part of your jaw is moved forward from the facial bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely.
This surgery may require the cooperation of an oral surgeon and an orthodontist. There are situations where this surgery may be combined with another procedure to improve the chances of success.
Laser-assisted uvulopalatoplasty
Similar to the UPPP, the procedure is performed with specialized equipment.
Tonsillectomy
Removal of the tonsils that can obstruct the upper airway. This is commonly done on children to improve symptoms of OSA.
Tracheostomy
This is reserved for times when other treatments have failed, and you have severe, life-threatening sleep apnea. In this procedure, your surgeon makes an opening in your neck and inserts a plastic tube through which you breathe. You keep the opening covered during the day, but at night you will uncover it to breath.
Worried you have sleep apnea? We’re here to help. Ask your primary care provider for a referral to the Salem Health Sleep Center.