Sepsis audit results for FY2020
08 Dec 2019Learn about diagnoses clinically validated in the records
By: Melissa Rodriguez, clinical documentation and coding specialist; and Jacqueline Smith, RN, clinical documentation improvement manager
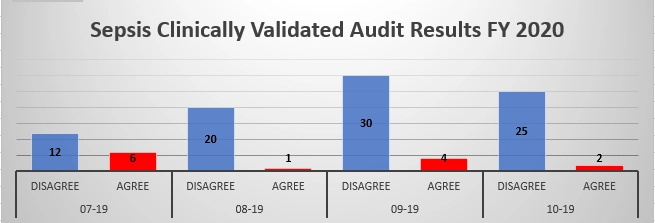
The chart below shows our sepsis audit results received in fiscal year 2020 for discharges from Sept. 28, 2018 to June 21, 2019.
The focus of the audit was to determine whether the diagnoses were clinically validated in the records. Auditors looked for the following in the medical record:
- Was the diagnoses clinically supported in the documentation through diagnostic findings, i.e. labs, radiology, etc. and linked to the diagnoses of sepsis?
- Did symptoms presented by the patient and documented by the provider support the diagnoses? (e.g. PE states “A&O x3” but the diagnoses in the plan says “encephalopathy.”)
- Was the diagnoses treated or monitored?
- Was the diagnoses consistently documented throughout the patient’s admission?
- Was the sepsis ruled out and documented that way
Below is the breakdown of the thirteen charts that did not meet clinical validation based on the above criteria:
- 5 met SH’s standard sepsis definition. Did not meet auditors’ sepsis clinical validation parameters (sepsis 3).
- 4 did not meet SH’ standard sepsis definition and were not consistently documented.
- 4 were unrelated to a sepsis diagnoses, but those diagnoses did not meet their own clinical validation.
Our recommendation is to clearly and consistently document the diagnoses of sepsis as defined by Salem Health’s standard definition. State what diagnostic findings or symptoms are supporting the diagnoses and link any treatments clearly. If the diagnoses is ruled out, it is OK and recommended to state so; it may even save a query from being generated.
If you have any questions about these results, please call Jacqueline Smith at 806-790-3415.