Open Payments—Time to review, dispute and correct
07 Jul 2019CMS Publishes Open Payments program 2018 data
By: Sue Kathy Xiong, MHA, CHC, Corporate Integrity & Safety manager
Centers for Medicare & Medicaid Services (CMS) published Open Payments data, along with newly submitted and updated payment records for previous program years.
For 2018, applicable manufacturers and group purchasing organizations (GPOs) collectively reported $9.35 billion publishable payments and ownership and investment interests to physicians and teaching hospitals.
In Oregon, more than 50% of the payments were compensation for services serving as faculty or as a speaker at a venue and consulting fees, as indicated in the pie chart below.
What is Open Payments?
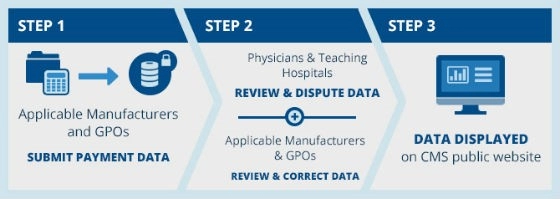
Open Payments is a national disclosure program that promotes transparency and accountability by making information about the financial relationships between applicable manufacturers and GPOs, and physicians and teaching hospitals available to the public. Through this program, the public has access to a more transparent and accountable health care system. Since the Open Payments program began in 2013, CMS has published 64.77 million records, accounting for $43.22 billion in payments and ownership and investment interests.
Recommended action
The Open Payments Program Year 2018 data and any newly submitted records are now available for review. As a physician, your review of the data is strongly encouraged. Review and Dispute activities are from April 1 until end of the calendar year. To learn how to register, review, and dispute your financial data, go to the Open Payments Physician and Teaching Hospital Review, Dispute and Correction website at www.openpaymentsdata.cms.gov/.
Questions? Concerns?
Contact the Corporate Integrity Department — Ellen Hampton 503-814-2828 or Sue Xiong, 503-814-2826.
Resources
Openpaymentsdata.cms.gov. (2019). [online] Available at: https://openpaymentsdata.cms.gov/summary-by-state [Accessed 28 Jun. 2019].