From IS: Automatic info added to discharge assessment
05 Jan 2020New automatic note under the Discharge Summary tab
By: Jeremy Bogan, information services business relations administrator
To comply with the new Centers for Medicare and Medicaid Services requirement, information will automatically pull into the D/C summary documents that contain Care Plan Information. When you create a new note under the Discharge Summary tab, the required text will now auto-populate (see screenshot below). This addition begins Jan. 1, 2020.
This note will have been entered by the care manager — so if the patient didn’t need care management help, just leave the template blank or delete it. If you have questions, please contact Drew Clarke, MD, at g.andrew.clarke@salemhealth.org.
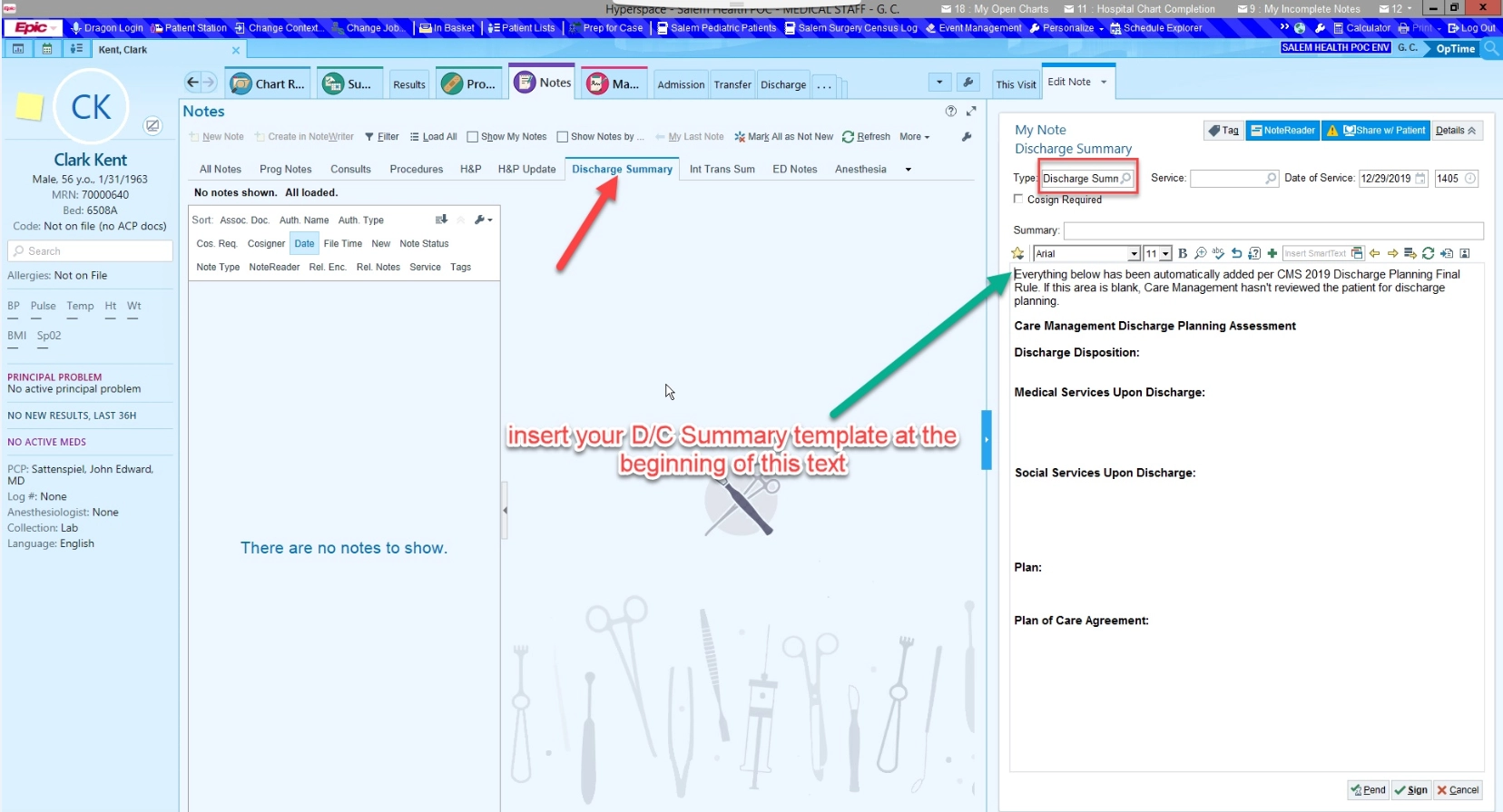
(Tip: Right click on the image above and select Open in new tab to enlarge the screenshot.)